Moments That Make the Beat Go On: Part I
Moments That Make the Beat Go On: Part I
by Chidera Alim
Introduction
Your heart is a remarkable organ for several reasons. Other than keeping you alive, the heartbeat can reflect attention, emotions and cognitive effort. Plus, your heart keeps beating while you’re resting and continues to beat for hours even when removed from the body. The heart drives blood flow to all organ systems, delivering oxygen and collecting waste to maintain homeostasis. The basis for this blood flow results from contraction of the heart, and each heartbeat results from the combined effort of several ions and proteins, especially calcium.

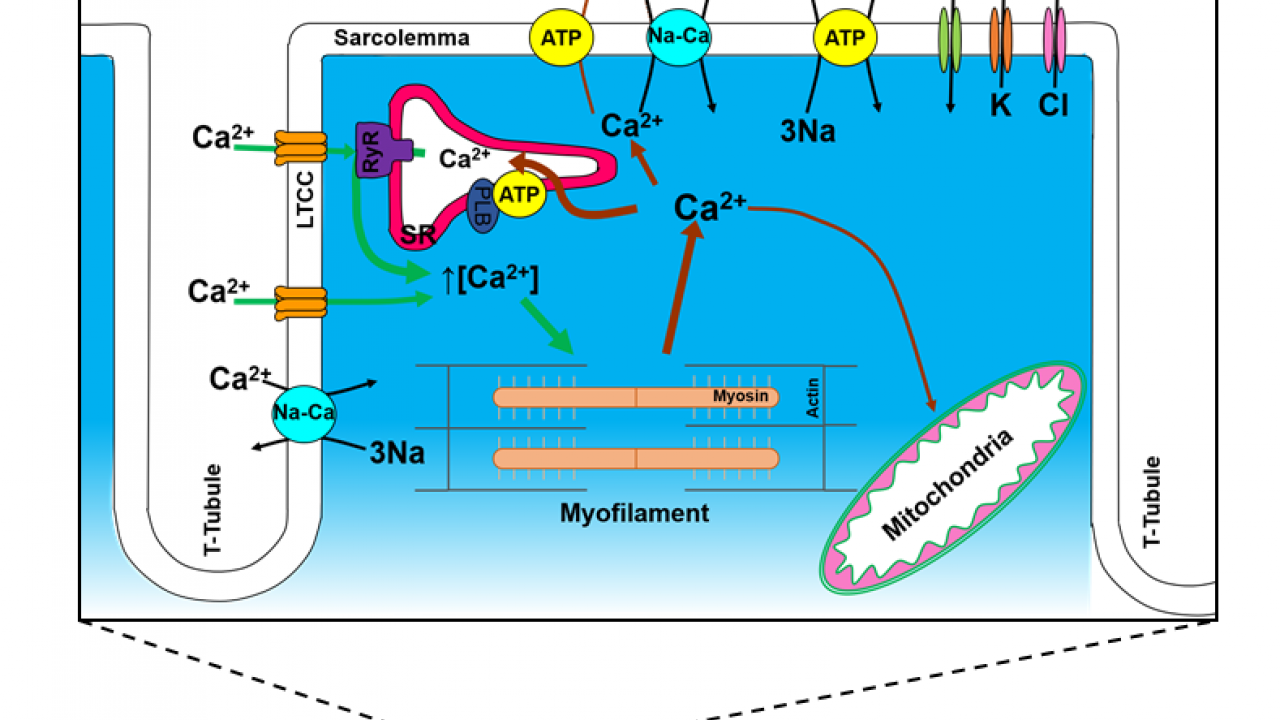
When you think of the functions of calcium, you probably think healthy bones and maybe blood clot, but calcium is extremely essential for every heartbeat in a healthy heart. Calcium (Ca2+) is a ubiquitous molecule that regulates several physiological processes in general, and the cardiovascular contractile system specifically. In summary, Ca2+ flows into the heart cell and triggers the release of even more Ca2+ from our intracellular Ca2+ store (the sarcoplasmic reticulum or SR). Now at a high concentration, Ca2+ binds Troponin which switches on the contractile machinery and the heart contracts. For relaxation to occur, free Ca2+ levels in the cytosol must decrease - this requires Ca2+ transport by pumps or exchangers (Donald M. Bers, 2002). Ca2+ unbinding from troponin shuts down the contractile machinery and a heartbeat is complete.
You might have learned about action potentials in neurons - influx of Na+ leading to depolarization and efflux of K+ leading to repolarization - electrical signals help stimulate a muscle to contract. Unlike in neural cells and even skeletal muscle cells, Ca2+ plays a role in the depolarization of heart cells or cardiomyocytes (Figure 1). This electrical activity followed by contraction is referred to as Excitation-Contraction Coupling.

Cardiac Excitation-Contraction Coupling (EC Coupling)
This term refers to the process from electrical excitation of the cardiomyocyte during the action potential (AP) and the resultant mechanical contraction in response which leads to the ejection of blood. Cardiomyocytes are either force producing/contractile cells or part of the electrical conduction system/autorhythmic cells. Only about 1% of heart cells make up the conduction system while 99% are contractile.

Mechanical Activity in the Heart
The striated appearance of cardiomyocytes (Figure 2a) is due to alternating thick (myosin) and thin (actin) filaments. These contractile protein filaments make up a sarcomere. In resting state, tropomyosin blocks the actin binding site (preventing myosin from binding actin). For contraction to occur, Ca2+ binds troponin, which “unlocks” tropomyosin and allows for actin and myosin to interact. The sliding of actin and myosin past each other results in contraction. When Ca2+ levels drop, the troponin-tropomyosin complex returns to its inhibiting position on the active site of actin. Contraction ends as the actin filaments return to their initial position, relaxing the muscle. When Ca2+ concentrations increase again, the cycle repeats. These cycles require energy. Cardiac cells contain numerous mitochondria, which enable continuous aerobic respiration and production of adenosine triphosphate (ATP) for cardiac function (Fawcett & McNutt, 1969). It’s important to note that Ca2+ is the direct activator of the myofilaments which cause contraction.
Electrical Activity in the Heart
Cardiac muscle is autorhythmic; it is capable of generating its own rhythmic electrical activity, referred to as pacemaker potentials. Pacemaker potentials involve several voltage gated channels including F-type Na+ channel (F: funny), T-type Ca2+ channel (T: transient), L-type Ca2+ channel (L: long lasting) and K+ channels. Pacemaker cells are grouped into specialized regions called nodes that together control the rate and coordination of cardiac contractions (Figure 2b):
- The sinoatrial (SA) node: primary pacemaker, drives the activity of other pacemaker structures in the heart with approximately 70 AP/min.
- The atrioventricular (AV) node: follows the faster SA node and exhibits autorhythmicity of 50 AP/min.
- The interatrial pathway: a pathway of specialized cells that conduct pacemaker activity from the right atrium to the left atrium.
- The internodal pathway: a pathway of specialized cells that conducts pacemaker activity from the SA node to the AV node.
- The Bundle of His: a conductive tract that originates at the AV node, divides and projects into the left and right bundles and ventricles.
- Purkinje fibers: small terminal fibers of specialized pacemaker cells that extend from the Bundle of His and spread throughout the ventricular myocardium. They exhibit auto-rhythmicity of 30 AP/min. Importantly, under normal conditions, all cells in the conduction system follow the SA node at 70 AP/min.


The pacemaker cells induce action potentials, which are conducted via the conduction pathways listed above, to the cardiac myocyte and induce contraction. During the cardiac action potential (Figure 3), membrane depolarization opens the Long-lasting Calcium channel allowing the influx of Ca2+ which induces the release of more intracellular Ca2+ (CICR) from the SR via the type-2 ryanodine receptors (RyR). This transient rise in free intracellular Ca2+ leads to cardiac contraction. Ca2+ is then transported out of the cytosol via SR Ca2+ pumps, sarcolemmal Na+↔️Ca2+ exchanger, sarcolemmal Ca2+ pumps or mitochondrial Ca2+ uniporter for relaxation to occur. Given the significance of Ca2+ in the heart, disturbance to the Ca2+ handling machinery could be detrimental and ultimately lead to heart failures and arrhythmias. Cardiovascular disease is the leading cause of death in the world at large. Hence, it is important to investigate calcium cycling and signaling in the heart. This opens up to a new field of study: Calcium dynamics.

References
Bers DM. Cardiac excitation–contraction coupling. Nature. 2002 Jan;415(6868):198-205.
Fawcett DW, McNutt NS. The ultrastructure of the cat myocardium: I. Ventricular papillary muscle. The Journal of cell biology. 1969 Jul 1;42(1):1-45.
