Microbiome Biotechnology: Challenges and Promise for the Future
Microbiome Biotechnology: Challenges and Promise for the Future
by Zach Bendiks
In recent years we have seen an explosion of news articles and public interest in the “microbiome”, to the point where Forbes magazine called the period between 2010-2019 “The Decade of the Microbiome”. Not only has the public become increasingly interested in this exciting area of research, but scientists are now using our understanding of the microbiome to create new technologies and services that promise to benefit human health. In this article, we will briefly explore what the microbiome is, how biotechnology is using our understanding of the microbiome, and current challenges that the field faces.
The human microbiome contains ~10 trillion bacteria cells, meaning there are roughly as many bacteria cells living in and on your body as there are human cells. These bacteria represent ~1,000 unique species who collectively contain ~2,000,000 genes, which is 100 times greater than the number of genes in the entire human genome. Importantly, the structure of the microbiome, such as the overall diversity or the abundance of specific bacterial species, has been associated with numerous health outcomes affecting the immune, cardiovascular, respiratory, and nervous systems. This has changed our understanding of human nutrition and health, and microbiome analysis could be used to determine a person’s likelihood of developing diseases or predict their response to drug or diet interventions and usher in a new era of personalized medicine. Because of its importance to various functions throughout the human body, the microbiome has been referred to as our “forgotten organ.”
The past decade has seen a sharp increase in the number of companies utilizing our understanding of the microbiome to develop new therapies or diagnostic tools. For example, the San Francisco-based company Second Genome, founded in 2010, has identified a protein produced by the microbiome that promotes healing of damaged intestinal surfaces and could be useful in treating patients with inflammatory bowel disease. The company is currently performing pre-clinical studies of this protein with the hopes of transitioning to clinical development in 2021. Other companies, such as Viome and Thryve, perform microbiome analyses on samples obtained from the customer’s own body, and provide detailed analyses of which microbes are present, what these microbes are doing, and even offer personalized nutrition and supplement recommendations based on the results. Earlier this year, Johnson & Johnson, one of the largest companies in America, partnered with Kaleido Biosciences to develop therapies that prevent the development of childhood allergies using bacteria from the human gut. These represent just some of the exciting new players in the biotechnology landscape, and there are dozens of new microbiome-focused companies appearing every year.

Challenges for Microbiome Biotechnology
One of the fundamental questions in microbiome research is the issue of causation. We have all heard the phrase “correlation does not imply causation” when discussing statistics, but this idea is of equal importance to microbiome research. While scientists have identified several correlations between microbiome composition and human health, relatively few studies have shown causation between the two, even though this question is of fundamental importance. For any microbiome-health association there are at least three possibilities that must be considered (Figure 1):
- Does a specific microbiome composition cause a specific health outcome? One example would be the bacterium Helicobacter pylori which can cause stomach ulcers.
- Does the health outcome cause the microbiome to take on a specific composition?
- Does a third factor, such as lifestyle choices or genetic factors, cause both the microbiome composition and the health outcome? An example would be an individual consuming a high-calorie diet, which can lead to obesity as well as changes in one’s microbiome.
It is important to note that these scenarios are not mutually exclusive, and in fact, these three factors can reinforce each other. For example, a landmark publication showed that microbiomes from obese mice extract more energy from the diet than microbiomes from lean mice, which demonstrates that the “obese microbiome” can reinforce obesity in the host.
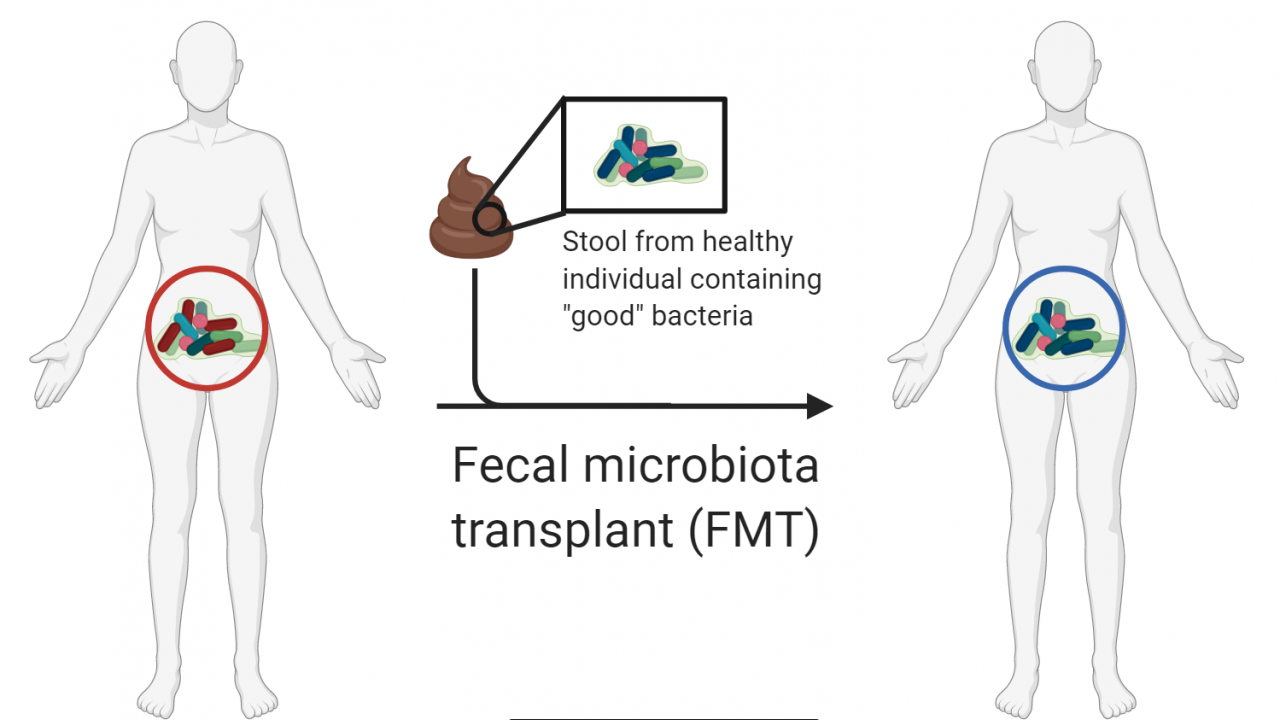
Much effort has been put into altering the composition of the microbiome to improve host health. If the microbiome is the causal agent for a disease state, then we would expect therapies targeting the microbiome to alleviate the disease. An example of this is fecal microbiota transplants (FMT), where the feces from a “healthy” person are given to a “sick” person, thus transferring the “healthy” microbiome to the patient, with the goal of eliminating the disease state (Figure 2). FMT has been used to treat Clostridioides difficile infections with great success and numerous research groups and biotechnology companies are exploring the applications of FMT to treat other diseases caused by the microbiome. However, we would not expect these interventions to be as effective in treating a disease if the microbiome is not the cause but is rather a symptom of the disease or is just one of several causes. Also, it is difficult to define what exactly a “healthy” microbiome is. Microbiomes exhibit a lot of variation between individuals, and these differences are even more apparent when comparing individuals from different countries and cultures. One can define a microbiome based on taxonomy (who is there?), function (what is the microbiome doing?), ecological succession (who appears when?), or community dynamics (does the microbiome recover from disturbances?), and as of now there is no consensus regarding how a healthy microbiome should be defined.

Looking Forward
Microbiome research has brought in a wave of new therapies and technologies, such as FMT, that are revolutionizing medicine and our understanding of human health. It is truly remarkable how much the field has grown in just the past 10 years, and the upcoming decade promises even more breakthroughs as computational power, funding, and study designs improve. An improved understanding of the microbiome’s role in the development of different diseases will be vital for creating improved therapies and technologies. One of the most exciting areas to watch moving forward is the gut-brain axis, which is the connection between the gut microbiome, the gastrointestinal tract, and host cognition. It is increasingly understood that the microbiome influences production of the neurotransmitters serotonin and tryptophan, which have a big impact on our perception and mood. There currently over 40 programs that are using our understanding of the gut-brain axis to develop treatments for depression, autism, and other cognitive disorders. Microbiome biotechnology represents the frontier of science, and the future looks extremely promising!
References
Carmichael, Taylor. “Johnson & Johnson To Collaborate With Microbiome Biotech On Childhood Allergies.” The Motley Fool, https://www.fool.com/investing/2020/01/09/johnson-johnson-to-collaborate-with-microbiome-bio.aspx.
Cat, Linh Anh. “The Decade Of The Microbiome.” Forbes, https://www.forbes.com/sites/linhanhcat/2019/12/31/decade-of-the-microbiome/#5163684c9961.
Fischbach, Michael A. “Microbiome: Focus on Causation and Mechanism.” Cell, vol. 174, no. 4, Elsevier Inc., 2018, pp. 785–90, doi:10.1016/j.cell.2018.07.038.
Gilbert, Jack A., et al. “Current Understanding of the Human Microbiome.” Nature Medicine, vol. 24, no. 4, 2018, pp. 392–400, doi:10.1038/nm.4517.
Gosalbez, Luis. “The Microbiome Biotech Landscape: An Analysis of the Pharmaceutical Pipeline.” Microbiome Times, https://www.microbiometimes.com/the-microbiome-biotech-landscape-an-analysis-of-the-pharmaceutical-pipeline/.
Grinspan, Ari. “FMT for Severe C. Difficile Infection: If at First You Do No Harm, the Second Time’s a Charm.” Digestive Diseases and Sciences, 2020, doi:10.1007/s10620-020-06309-z.
Kashyap, Purna C., et al. “Microbiome at the Frontier of Personalized Medicine.” Mayo Clinic Proceedings, 2017, doi:10.1016/j.mayocp.2017.10.004.
Lloyd-Price, Jason, et al. “The Healthy Human Microbiome.” Genome Medicine, 2016, doi:10.1186/s13073-016-0307-y.
Nie, Pengqing, et al. “Gut Microbiome Interventions in Human Health and Diseases.” Medicinal Research Reviews, vol. 39, no. 6, 2019, pp. 2286–313, doi:10.1002/med.21584.
O’Mahony, S. M., et al. “Serotonin, Tryptophan Metabolism and the Brain-Gut-Microbiome Axis.” Behavioural Brain Research, 2015, doi:10.1016/j.bbr.2014.07.027.
Second Genome Pipeline. https://www.secondgenome.com/pipeline.
Sender, Ron, et al. “Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans.” Cell, vol. 164, no. 3, Elsevier Inc., 2016, pp. 337–40, doi:10.1016/j.cell.2016.01.013.
Turnbaugh, Peter J., et al. “An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest.” Nature, vol. 444, no. 7122, 2006, pp. 1027–31, doi:10.1038/nature05414.
